Physiotherapy Treatment for Swan Neck Deformity: Exercises, Splints, and Rehab Guide
What is Swan Neck Deformity?
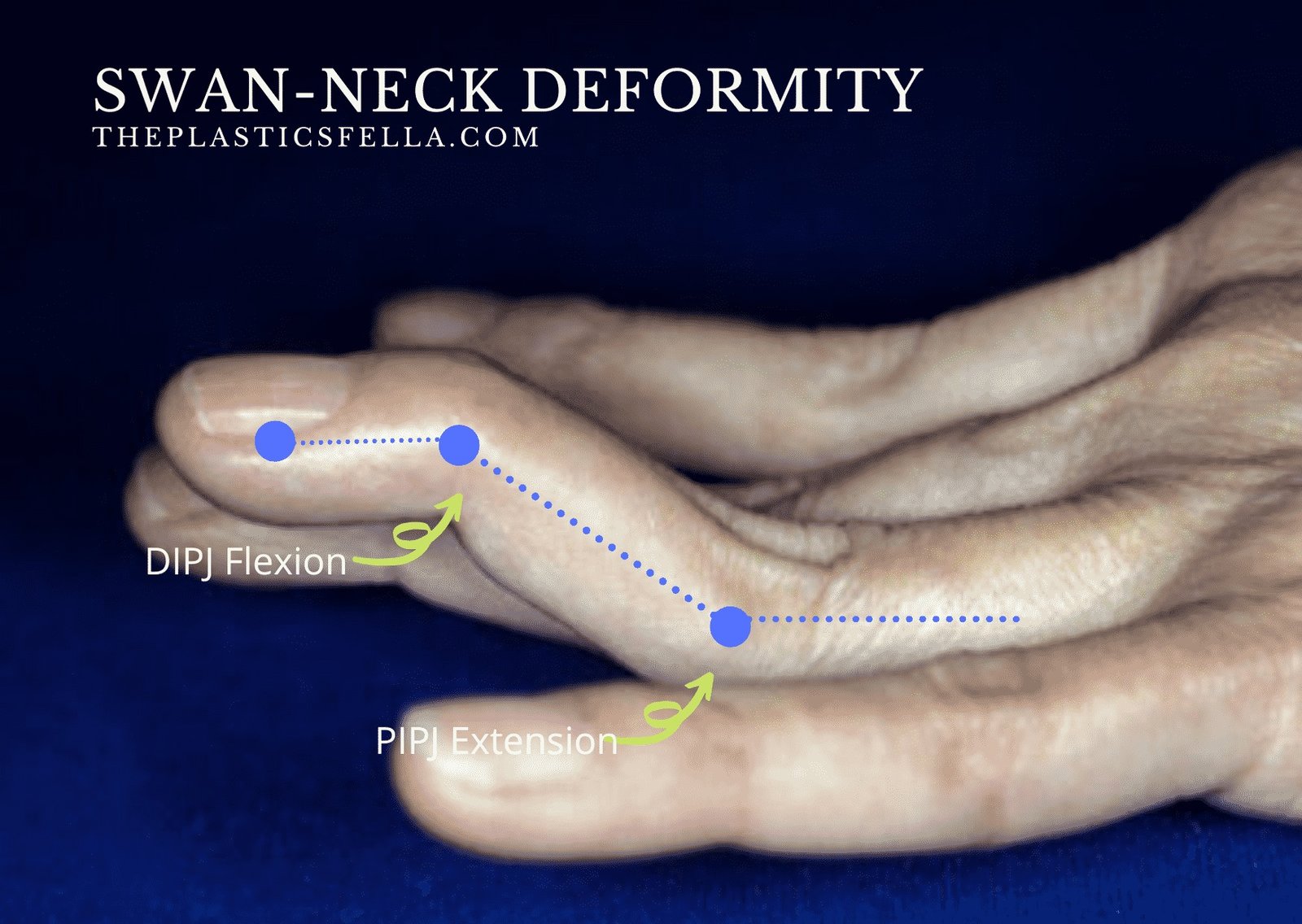
Swan neck deformity refers to a specific pattern of joint dysfunction in the fingers. The classic features include:
- Hyperextension of the PIP joint (the middle joint of the finger)
- Flexion of the DIP joint (the joint closest to the fingertip)
- In more advanced cases, a secondary involvement of the metacarpophalangeal (MCP) joint may occur
This deformity can make it difficult to grip, pinch, or hold objects and often results in visible finger misalignment.
Causes of Swan Neck Deformity
Swan neck deformity can result from various underlying conditions. Some of the most common causes include:
Rheumatoid Arthritis (RA)
RA is the most common cause of swan neck deformity. Chronic inflammation of the synovial membrane leads to ligament laxity, joint capsule stretching, and tendon imbalance.
Trauma or Injury
Injury to the volar plate (a thick ligament on the palmar side of the PIP joint) or extensor mechanism can cause the PIP joint to hyperextend, leading to deformity.
Laxity or Looseness of Ligaments
In people with Ehlers-Danlos syndrome or other connective tissue disorders, ligament laxity may contribute to joint instability and deformities such as swan neck.
Neurological Conditions
Diseases like cerebral palsy or Parkinson’s disease may lead to muscle imbalance and joint dysfunction, resulting in finger deformities.
Mallet Finger
An untreated or improperly healed mallet finger can lead to a secondary swan neck deformity due to compensatory changes in tendon tension.
Symptoms of Swan Neck Deformity
The primary symptom of swan neck deformity is a noticeable bend in the finger joints. Other signs and symptoms include:
- Difficulty straightening or bending the finger
- Weak grip strength
- Pain or discomfort in the affected finger
- Swelling around the PIP joint
- Loss of hand function in severe cases
These symptoms may worsen with time if left untreated, especially if the underlying cause is progressive, like rheumatoid arthritis.
Diagnosis
Diagnosing swan neck deformity involves a physical examination and a detailed medical history. A physician will assess the range of motion, joint alignment, and flexibility of the finger. Diagnostic tools may include:
- X-rays: To examine joint damage or misalignment
- MRI or Ultrasound: To assess soft tissue structures like tendons and ligaments
- Blood Tests: In cases where autoimmune disease like RA is suspected
Early diagnosis is crucial to prevent permanent joint damage and loss of function.
Read more: Carpal Tunnel Syndrome (CTS): Causes, Symptoms, Diagnosis, and Treatment
Treatment Options for Swan Neck Deformity
Treatment depends on the underlying cause, severity, and functional impairment. Options range from conservative management to surgical intervention.
- Non-Surgical Treatments
- Splinting
Custom hand splints or orthoses help in stabilizing the PIP joint and preventing hyperextension. These are especially useful in early stages.
- Physical Therapy
Hand therapy with exercises to strengthen intrinsic hand muscles can improve balance and function. Therapists may also use heat, ultrasound, or massage to relieve pain and stiffness.
- Medications
In cases caused by rheumatoid arthritis or inflammation:
- NSAIDs (Non-steroidal anti-inflammatory drugs)
- DMARDs (Disease-modifying antirheumatic drugs)
- Steroid injections
- Occupational Therapy
Therapists assist patients with adaptive techniques and tools for daily activities, improving hand function and reducing strain.
- Surgical Treatments
Surgery is considered when non-invasive treatments fail or deformity significantly impairs function. Surgical options include:
- Soft Tissue Procedures
These include tendon repair, lateral band relocation, or volar plate advancement.
- Joint Fusion (Arthrodesis)
In severe cases, the DIP joint is fused to relieve pain and stabilize the finger.
- Joint Replacement (Arthroplasty)
For patients with joint destruction, artificial joint replacement may be a viable option.
- Boutonniere Correction (If Present Simultaneously)
Correcting overlapping deformities like boutonniere deformity may also be necessary.
Recovery and Prognosis
The prognosis of swan neck deformity depends on the timing of treatment and the underlying condition. Early detection often results in better outcomes. With proper management, many patients regain functional use of their hand and experience significant symptom relief.
Surgical recovery may involve several weeks of immobilization followed by rehabilitation. Hand therapy plays a crucial role in regaining strength and mobility post-surgery.
Prevention Tips
While not all causes of swan neck deformity are preventable, certain strategies can reduce the risk:
- Manage chronic conditions like rheumatoid arthritis with regular follow-ups
- Avoid repetitive stress injuries to the hands
- Use protective gear during sports or high-risk activities
- Perform hand stretching and strengthening exercises regularly
- Treat mallet finger or ligament injuries promptly to avoid progression
Physiotherapy Treatment for Swan Neck Deformity
Physiotherapy plays a vital role in the conservative management of swan neck deformity, especially in the early stages or in patients who are not candidates for surgery. The primary goals are to improve joint stability, prevent progression, restore function, and minimize pain.
A physiotherapist uses a combination of manual therapy, custom splinting, therapeutic exercises, and education to optimize outcomes.
🔍 Goals of Physiotherapy Management
- Prevent further joint deformity
- Reduce inflammation and pain
- Improve hand strength and dexterity
- Maintain flexibility of the interphalangeal joints
- Educate the patient on joint protection strategies
🧤 1. Splinting and Orthotic Management
Custom finger splints are often the first line of defense. They help control joint positioning and prevent hyperextension of the PIP joint. Common types include:
- Ring splints (SilverRing™ or Oval-8™): Help maintain the PIP joint in a neutral or slightly flexed position
- Figure-8 splints: Stabilize both the PIP and DIP joints
- Dynamic splints: Allow controlled movement and prevent contractures in more severe cases
Splinting is usually combined with exercise therapy for optimal results.
🧘 2. Therapeutic Exercises
Physiotherapists use targeted exercises to improve the balance of finger extensor and flexor muscles, especially the lumbricals and interossei. Exercises should be tailored to each patient, depending on joint mobility and stability.
- Tendon Gliding Exercises
These help maintain mobility of flexor tendons and prevent adhesions:
- Straight hand
- Hook fist
- Full fist
- Tabletop position
- Straight fist
➡️ Reps: 10 reps, 3 times daily
- Intrinsic Muscle Strengthening
Weakness in the intrinsic muscles can worsen deformity. Strengthening exercises include:
- Putty squeezing
- Rubber band resistance (finger abduction)
- Finger “O” formations with resistance
➡️ Focus on gentle isometric exercises in early stages.
- Joint Range of Motion (ROM) Exercises
To prevent joint stiffness and promote flexibility:
- Passive flexion of the PIP joint
- Active DIP joint extension
➡️ Always avoid forceful extension of the PIP joint to prevent worsening of hyperextension.
💆 3. Manual Therapy
Manual techniques may be used to:
- Improve joint alignment
- Reduce soft tissue tightness
- Address extensor mechanism imbalances
Techniques may include:
- Joint mobilizations (grade I–II) for pain and gentle movement
- Soft tissue massage around the volar plate or lateral bands
- Myofascial release to address tight fascia or scar tissue
🔥 4. Modalities (Electrotherapy)
Electrotherapy may be used to manage inflammation, pain, or soft tissue tightness.
- Ultrasound Therapy: Promotes tissue healing and reduces fibrosis
- TENS (Transcutaneous Electrical Nerve Stimulation): For pain management
- Paraffin Wax Bath: Increases circulation and joint flexibility before exercises
🧑🏫 5. Patient Education and Joint Protection
Education is one of the most powerful tools in physiotherapy. Patients need to understand how to protect their joints during daily activities.
Key education points:
- Avoid activities that cause PIP joint hyperextension
- Use assistive tools (jar openers, ergonomic pens, etc.)
- Practice joint protection techniques (e.g., using larger joints like the elbow or shoulder instead of fingers for tasks)
- Encourage regular breaks during repetitive hand tasks
- Emphasize importance of compliance with splint use and exercise regimen
🩺 6. Multidisciplinary Approach
A physiotherapist may work alongside:
- Occupational therapists, who help with adaptive devices and fine motor coordination
- Rheumatologists, in cases caused by autoimmune conditions
- Orthopedic or hand surgeons, if deformity progresses or surgical intervention is considered
📅 Sample Physiotherapy Plan (6 Weeks)
| Week | Focus | Interventions |
| 1–2 | Pain reduction, splinting, ROM | Splint fitting, passive ROM, wax bath |
| 3–4 | Strength and control | Isometric exercises, tendon gliding |
| 5–6 | Function and independence | Intrinsic strengthening, task simulation, joint protection training |
✅ Outcome Measures
To monitor progress, physiotherapists often use:
- DASH Score (Disabilities of the Arm, Shoulder, and Hand)
- Grip strength tests
- Range of motion (goniometric measurement)
- Pain scales (VAS)
Regular reassessment ensures that treatment goals are being met and the plan can be adjusted as needed.








